Splanchnic Nerve Block and Radiofrequency Ablation - Asian Pain Academy
- Asian Pain Academy

- Sep 24, 2025
- 9 min read

1. Introduction
The splanchnic nerve block is an advanced image-guided intervention targeting the preganglionic sympathetic fibers responsible for transmitting visceral nociceptive signals from the upper abdominal organs. These nerves are part of the thoracic sympathetic chain and represent an important relay in the pain pathway from organs such as the pancreas, liver, stomach, and adrenals.
The block is performed at the T11–T12 vertebral level via a posterior paraspinal approach, most commonly under fluoroscopic guidance, though CT or ultrasound may also be used in selected situations.
When extended relief is desired, especially in patients with chronic pancreatitis or intractable upper abdominal cancer pain, radiofrequency ablation (RFA) of the splanchnic nerves is performed. It offers a controlled, predictable, and repeatable lesioning method with a favorable safety profile.
This technique is particularly valuable in cases where the coeliac plexus is inaccessible or anatomically distorted due to tumors or prior surgery. Additionally, the splanchnic nerve block has become a preferred option when coeliac neurolysis carries elevated vascular risk or has previously failed.
2. Anatomy of the Splanchnic Nerves
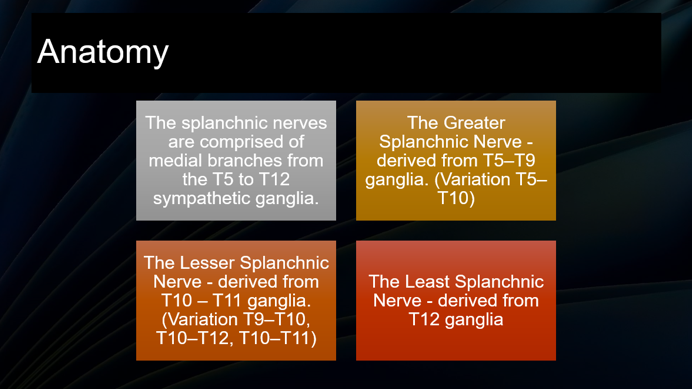
The thoracic splanchnic nerves are paired bundles of preganglionic sympathetic efferent fibers that emerge from the thoracic sympathetic trunk and descend anteromedially to join the prevertebral ganglia in the upper abdomen. They consist of:
Greater splanchnic nerve: Originates from the T5–T9 thoracic ganglia; the largest contributor; often targeted in interventional pain procedures.
Lesser splanchnic nerve: From T10–T11; provides sympathetic input to the aorticorenal and superior mesenteric plexuses.
Least (lowest) splanchnic nerve: From T12; contributes to renal plexus.
All three descend through the crura of the diaphragm and converge anterior to the T11–L1 vertebral bodies before synapsing in the coeliac ganglia, superior mesenteric plexus, and aorticorenal plexus.
These nerves carry afferent visceral pain signals from the following organs:
Stomach
Pancreas
Liver and gallbladder
Spleen
Adrenal glands
Small intestine up to mid-transverse colon
Omentum and peritoneal membranes
Knowledge of this anatomical pathway is necessary when choosing between a splanchnic nerve block and a coeliac plexus block for the relevant pain syndrome.
3. Indications for Splanchnic Nerve Block and RFA
A. Cancer-Related Visceral Pain
Pancreatic carcinoma: One of the most painful abdominal malignancies; often responsive to splanchnic neurolysis or ablation.
Gastric cancer: Especially when involving the retroperitoneum or coeliac axis.
Liver metastases, adrenal tumors, and peritoneal carcinomatosis
Retroperitoneal tumors compressing or invading the coeliac plexus
B. Non-malignant Chronic Visceral Pain
Chronic pancreatitis: Repeated splanchnic blocks or RFA help reduce opioid dependence and improve function.
Refractory upper abdominal pain syndromes: Including pain after biliary surgery or functional abdominal pain not responsive to pharmacotherapy.
Post-surgical neuropathic abdominal pain, when other somatic interventions fail.
C. Situations Where Coeliac Plexus Block is Contraindicated
Distorted anatomy due to tumors, radiation fibrosis, or post-surgical adhesions
High risk of bleeding or vascular injury near the aorta
Failed or incomplete pain relief from previous coeliac block
4. Rationale for Choosing Splanchnic Nerve Target
Compared to Coeliac Plexus Block:
Easier to access using a posterior paraspinal approach under fluoroscopy
Farther from major vessels like the aorta and inferior vena cava, reducing risk of vascular injury
Lower incidence of hypotension and diarrhea since preganglionic fibers are blocked upstream
Allows both chemical neurolysis (with alcohol or phenol) and radiofrequency ablation, providing short- and long-term pain relief
Ideal for image-guided RFA, with easily visible osseous landmarks and minimal anatomical distortion
5. Contraindications
Absolute Contraindications
Uncontrolled bleeding diathesis or anticoagulation
Local or systemic infection
Patient refusal
Allergy to contrast or local anesthetic agents
Relative Contraindications
Severe kyphoscoliosis or vertebral deformity obstructing posterior approach
Prior spinal instrumentation or surgery at T11–T12
Advanced pulmonary disease with intolerance to prone positioning
Inability to wean from high-dose vasopressors or in circulatory shock
6. Patient Preparation and Positioning
The patient is placed in the prone position on a radiolucent table. A small cushion or bolster may be placed under the abdomen to flatten the natural lumbar lordosis, which improves access to the thoracolumbar spine. The arms can be positioned overhead or alongside the body for patient comfort.
Standard monitoring (ECG, pulse oximetry, and non-invasive blood pressure) should be instituted, and an intravenous line must be secured. Preloading with crystalloids is often recommended, especially in cancer patients who may have autonomic instability or are scheduled for neurolytic procedures.
Fluoroscopic equipment should be positioned to allow clear visualization of both anteroposterior (AP) and lateral views of the T11 and T12 vertebral bodies, the target region for splanchnic nerve access.

7. Needle Insertion Technique: Fluoroscopy-Guided Approach

a. Landmarks and Needle Pathway
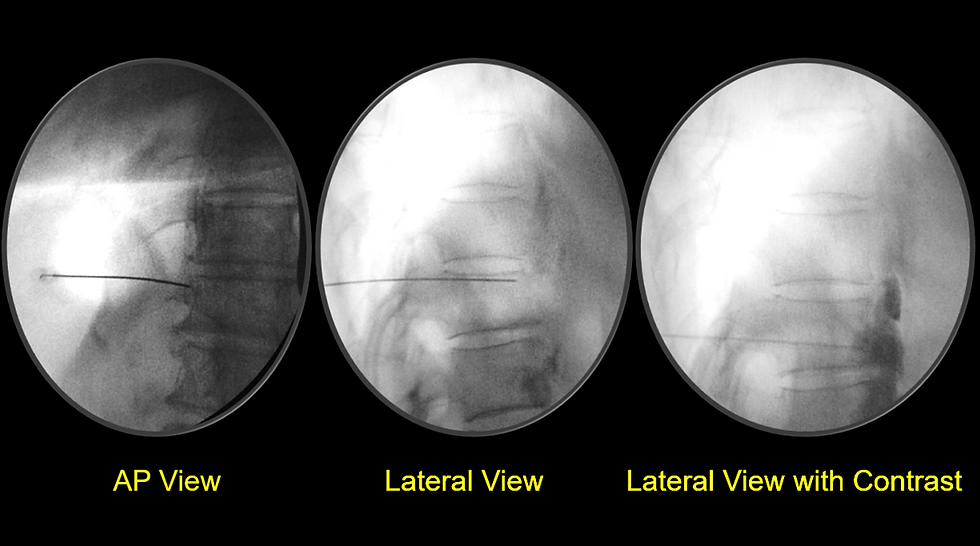
The target area is the anterolateral aspect of the T11 or T12 vertebral body, which corresponds to the path of the greater and lesser splanchnic nerves. The AP fluoroscopic view is used initially to identify the T11–T12 vertebral levels and the lateral edge of the vertebral body.
The needle entry point is located approximately 6–8 cm lateral to the midline, typically at the T11 or T12 transverse process level. Using a 22-gauge, 15 cm spinal needle, the operator directs the needle medially and slightly anteriorly toward the anterolateral corner of the vertebral body.
b. Needle Advancement and Depth Confirmation
As the needle approaches the vertebral body, the operator switches to a lateral fluoroscopic view to confirm the depth and avoid overshooting. The needle tip should lie just anterior to the vertebral body but posterior to the aorta or inferior vena cava, depending on the side. It should also remain retrocrural (behind the diaphragm).
After negative aspiration for blood or cerebrospinal fluid, contrast injection is performed to confirm proper spread and avoid intravascular or intrapleural injection.
8. Contrast Injection and Image Interpretation
A small volume of non-ionic contrast agent (usually 2–3 mL of iohexol) is injected through the needle under fluoroscopic guidance.
In the lateral view, contrast should outline the anterior surface of the vertebral body, forming a characteristic teardrop or comma-shaped pattern. This indicates correct retrocrural spread.
In the AP view, the contrast should appear as a bilateral or unilateral crescent adjacent to the vertebral column, without extension into epidural, vascular, or pleural spaces.
Care must be taken to avoid:
Vascular spread (contrast rapidly washes away or opacifies vessels)
Epidural spread (contrast tracks vertically along the spinal canal)
Pleural injection (contrast outlines lung borders)
If any of the above are suspected, the procedure should be reassessed before injecting therapeutic agents.
9. Drug Injection Protocols
a. Diagnostic and Therapeutic Blocks
For diagnostic or short-duration therapeutic blocks, the following drugs are commonly used:
0.25% Bupivacaine or 0.2–0.5% Ropivacaine: 5 to 8 mL per side
Dexamethasone 4–8 mg may be added to reduce post-block inflammation and prolong analgesia
The expected duration of pain relief is typically several hours to a few days, depending on the cause of the pain and the drug used.

b. Neurolytic Blocks for Malignant Pain
After confirming correct placement and administering a test dose of local anesthetic, neurolytic agents are administered:
Absolute alcohol (96%): 5 to 10 mL per side
Phenol (6–10%) in glycerin: alternative to alcohol, especially in patients with severe burning pain or risk of hypotension
Alcohol causes dehydration and necrosis of the nerve fibers, while phenol causes protein denaturation. Injection is performed slowly over 2–3 minutes, and patient vitals should be monitored continuously.

10. Radiofrequency Ablation (RFA) of Splanchnic Nerves

a. Indications
Radiofrequency ablation is a preferred option for non-cancer chronic visceral pain, especially in patients with:
Chronic pancreatitis
Abdominal pain syndromes with sympathetic dominance
Contraindications to neurolytic agents
Desire for a reversible and titratable pain intervention
b. Equipment and Cannula Placement
Radiofrequency generator
22-gauge RF cannula, 10–15 cm long, with 5–10 mm active tip
Stimulation-capable RF probes
Grounding pad securely attached to patient
Cannulas are placed bilaterally at the anterolateral surface of T11–T12 vertebral bodies, same as in conventional block. Fluoroscopy (AP and lateral views) is used for needle advancement and confirmation of position.
c. Sensory and Motor Testing
Sensory stimulation at 50 Hz: confirms that the electrode is in proximity to the target by reproducing the patient’s visceral pain or abdominal pressure.
Motor stimulation at 2 Hz: ensures no lumbar somatic nerve proximity (i.e., no lower limb muscle contraction).
d. Lesioning Parameters
After satisfactory stimulation results:
Inject 1 mL of 1% lignocaine to anesthetize the nerve
Perform thermal lesioning at 80°C for 90 to 120 seconds
Rotate cannula 5–10° to create overlapping lesions if needed
Repeat on the contralateral side
In selected cases, pulsed radiofrequency (42°C for 120 seconds) may be used to avoid nerve destruction while modulating pain transmission.

11. Post-procedure Monitoring
After the procedure, the patient is observed in a recovery area for at least 30 to 60 minutes. Monitoring includes:
Blood pressure and heart rate (hypotension is possible due to sympathetic blockade)
Pain assessment using numeric rating scale (NRS)
Neurological assessment (rule out leg weakness or unusual sensory changes)
Early ambulation once stable
Patients undergoing neurolysis should be counseled about possible delayed hypotension, diarrhea, and the potential need for repeat blocks if pain recurs.
12. Expected Outcomes and Duration of Relief
a. After Diagnostic or Therapeutic Block
Pain relief typically begins within 30 minutes and lasts from a few hours to several days, depending on the agent used.
Serves both as a therapeutic and prognostic tool to determine the likelihood of success with neurolysis or RFA.
b. After Neurolytic Block (Alcohol or Phenol)
Onset: within 1–6 hours, with peak analgesia over 24 hours.
Duration: generally ranges from 2 to 6 months, though certain patients may report extended periods of symptomatic relief.
Success rate: 60–90% of patients with upper abdominal cancer pain, especially pancreatic malignancy, report significant pain relief and reduced opioid use.
c. After Radiofrequency Ablation
Onset: gradual over several days.
The duration is generally between four and twelve months.
Especially beneficial in chronic pancreatitis and non-malignant visceral pain where repeat blocks are needed.
Outcome is influenced by:
The precision of needle placement.
Completeness of nerve destruction (in neurolysis).
Patient selection (visceral vs. somatic pain, tumor burden).
Co-existing psychiatric or central sensitization factors.
13. Complications and How to Avoid Them
a. Common and Expected Effects
Transient hypotension: Due to blockade of sympathetic vasoconstrictor fibers. Managed with fluids and vasopressors if needed.
Diarrhea: Caused by unopposed parasympathetic activity; generally self-limited.
Transient back or epigastric pain: Can occur during or after neurolysis.
b. Serious Complications
Vascular Injury or Hematoma
· Cause: Needle penetration of the aorta, vena cava, or lumbar arteries.
· Prevention: Lateral fluoroscopic views and contrast injection are recommended prior to neurolysis.
Pneumothorax
· Cause: Needle puncture of the pleura, especially with high thoracic insertions.
· Prevention: Keep needle trajectory below the rib cage and crura.
Spinal Cord Ischemia or Paraplegia (Rare but Severe)
· Cause: Damage to the artery of Adamkiewicz or anterior spinal artery, or neurolytic spread to neural structures.
· Prevention: Avoid midline or epidural spread, limit neurolytic volume, and always confirm contrast flow.
Urinary Retention or Constipation
· Cause: Autonomic imbalance.
Neurological Injury
· Cause: Direct needle trauma or excessive RF lesioning beyond the target zone.
· Prevention: Use motor stimulation and restrict RF lesion size and duration.
Infection or Abscess Formation
· Risk: Rare if strict aseptic precautions are followed.
Transient Leg Weakness or Numbness
· Cause: Inadvertent drug spread to lumbar plexus or psoas muscle.
14. Comparison with Other Visceral Pain Interventions
Feature | Splanchnic Nerve Block | Coeliac Plexus Block | Superior Hypogastric Block |
Target | Preganglionic thoracic nerves | Coeliac ganglia around aorta | Pre-sacral sympathetic plexus |
Pain type addressed | Upper abdominal visceral pain | Upper abdominal visceral pain | Pelvic visceral pain |
Anatomical complexity | Moderate | Higher (proximity to aorta, SMA) | High (deep pelvis) |
Vascular risk | Lower | Higher | Moderate |
Suitable for distorted anatomy | Yes | Often difficult | Variable |
RFA feasibility | Easy | Technically challenging | Moderate |
Splanchnic nerve block is commonly used when coeliac plexus block is contraindicated or presents a greater vascular risk, and is often indicated for patients with retroperitoneal masses.
15. Clinical Pearls
Always identify the visceral nature of pain before selecting a splanchnic block. It is not effective for somatic or neuropathic pain.
The lateral fluoroscopic view is more important than the AP view in confirming proper depth and avoiding aortic puncture.
In cancer patients, perform block early before high opioid dependence or severe cachexia limits outcomes.
For chronic pancreatitis, RFA offers a repeatable, reversible, and titratable modality.
Sensory and motor stimulation must be part of every RFA procedure to reduce the risk of neural injury.
Contrast spread patterns should be reviewed carefully before any permanent lesion is made.
Avoid neurolytic blocks in patients with central sensitization, coagulopathy, or uncontrolled sepsis.
About The Author of the Article Splanchnic Nerve Block and Radiofrequency Ablation
Dr. Debjyoti Dutta is a renowned Pain Physician and Faculty at the Asian Pain Academy, with extensive expertise in interventional pain management and ultrasound- and fluoroscopy-guided procedures. He has trained doctors across India and abroad, authored numerous academic resources, and is dedicated to advancing evidence-based pain medicine through education, innovation, and compassionate patient care.
.jpg)
Comments